OECD urges faster access and better use of resources in cancer care
Europe must improve access, reduce low-value care and put patients at the centre of cancer services, according to a new OECD report

Health systems across Europe need to deliver cancer care more quickly, more consistently and with greater focus on patients’ wider needs, according to a new report from the Organisation for Economic Co-operation and Development (OECD).
The report, ‘Delivering High-Value Cancer Care’, says that while survival rates have improved and mortality has fallen over the past two decades, rising numbers of cancer diagnoses are placing growing pressure on health systems, exposing persistent gaps in access, efficiency and quality of care.
In 2024, an estimated 2.7 million people were diagnosed with cancer across the European Union, equivalent to more than five new cases every minute, according to data from the European Cancer Information System. Although fewer people are dying from cancer, more are living with the disease, increasing demand for long-term treatment and support.
Drawing on policy surveys from 34 countries, international indicators and stakeholder consultations, the OECD identifies three priorities for improving the value of cancer care: timely access to services, evidence-based and efficient treatment, and people-centred approaches.
Delays and uneven access
The OECD warns that delays in diagnosis and treatment remain a major barrier to better outcomes. It calls for improved health literacy, targeted awareness campaigns and the removal of financial barriers that prevent people from seeking care early. More efficient screening and diagnostic pathways are also needed to reduce waiting times.
Access to clinical trials is also uneven, with patients in larger countries like France, Germany and Spain, far more likely to be enrolled than those in smaller states or in Central and Eastern Europe, limiting access to innovative treatments.
Gaps in quality and efficiency
Despite the importance of consistent clinical standards, only 12 EU+2 countries systematically monitor whether cancer care follows national guidelines, the report finds. Several countries are moving toward risk-stratified screening, using genetic, lifestyle or vaccination data to better target resources, but overdiagnosis remains a concern—particularly for thyroid and prostate cancers.
The OECD says updating screening and treatment guidelines, reducing low-value care and shifting services toward outpatient and day-surgery models could significantly improve efficiency. Nordic countries are highlighted as leaders in outpatient cancer care, while greater use of biosimilar medicines and stronger health technology assessment could help control costs.
Beyond the hospital
The report also stresses the importance of people-centred care. After-hours cancer services in Germany and Ireland, and the use of digital health tools in Greece and Sweden, are cited as examples of how access and continuity of care can be improved.
Cancer’s impact extends beyond health systems. Across OECD countries, a cancer diagnosis reduces the likelihood of employment by around 14%, underlining the need for better coordination between healthcare, social services and labour market policies.
Rising diagnoses among younger women
The OECD highlights a particularly worrying trend: rising cancer incidence among younger adults, especially women aged 15-49. Since 2000, cancer incidence has increased more rapidly among women than men. Between 2000 and 2022, age-standardised incidence rose by 10% among women, compared with 2% among men.
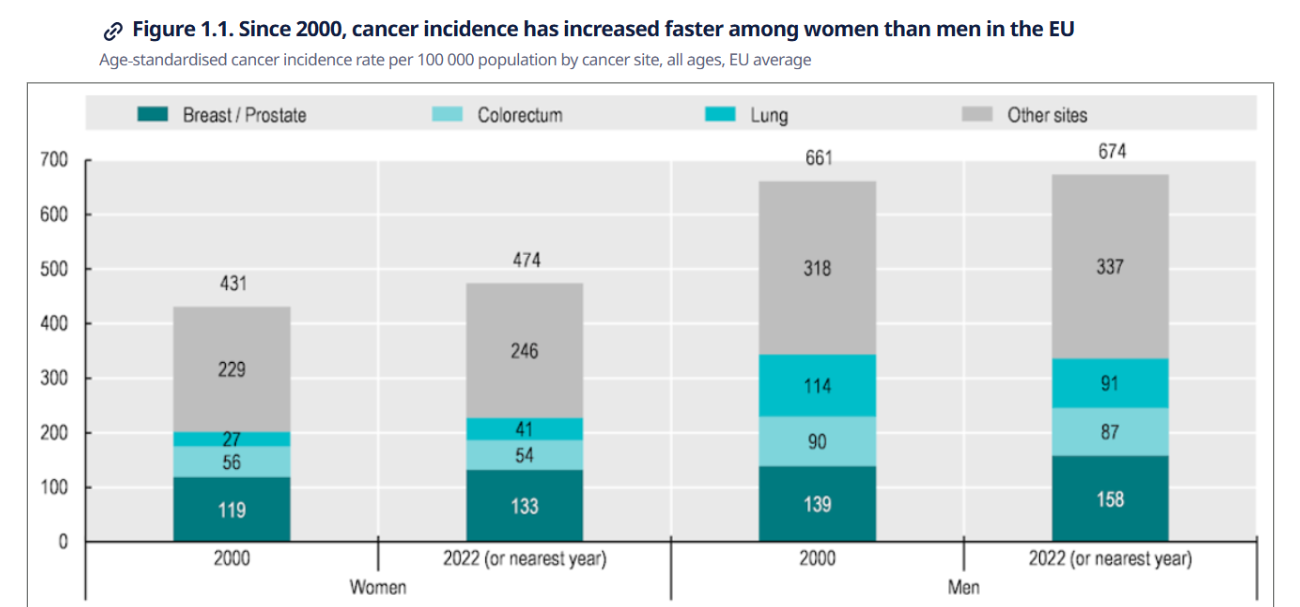
Over the same period, cancer mortality fell by 18% among women and 26% among men. However, mortality rates remain higher among men in every EU country, as well as in Iceland and Norway.
According to the OECD, these trends indicate that, while progress has been made in prevention and treatment, further reforms are needed to ensure that cancer care is delivered faster, more efficiently, and more equitably as demand continues to rise.
